Elephant’s Continually-updating Coronavirus Diary. ~ Waylon
~
We are starting to enter into a new normal.
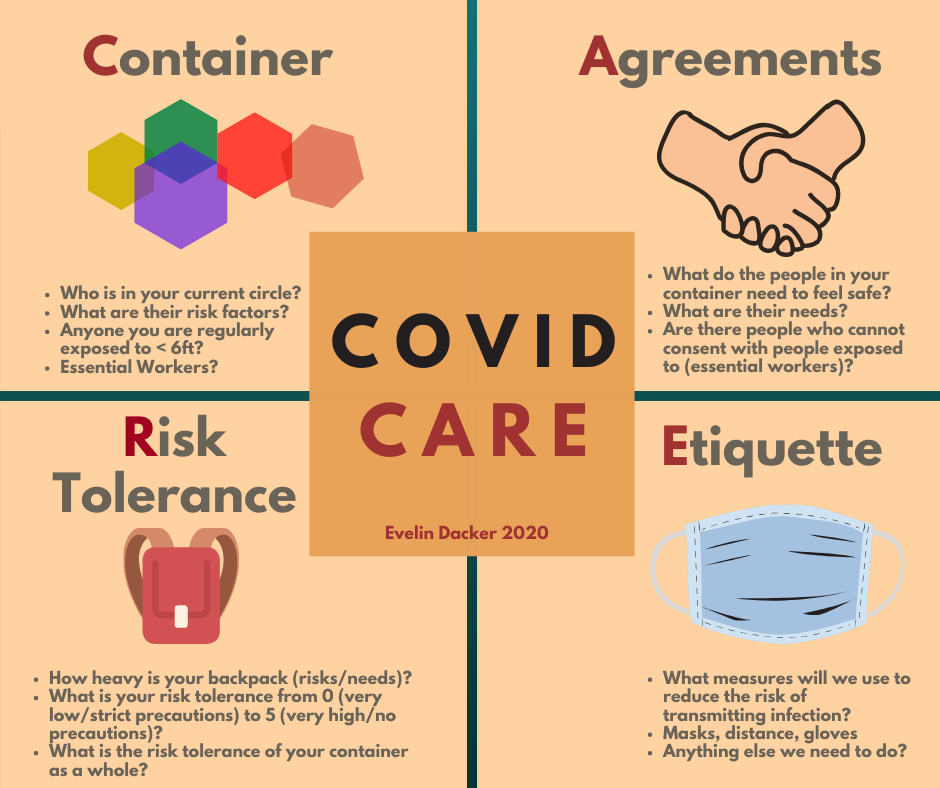
COVID CARE is a harm-reduction communication model that can guide us as stay-at-home measures are being lifted. Until accurate testing is available and herd immunity is achieved, we can lessen our harm to one another through self-awareness and communication.
COVID CARE calls in four specific elements to consider and discuss with others as you start broadening your social circles:
Container, Agreements, Risk Tolerance, and Etiquette.
In addition to discussing our individual risks, communication with others about our social circles, risk tolerance, and needs, will become necessary to lessen viral transmission. Rather than use shame and fear, meeting people where they are with compassion through the COVID CARE model, can help us cocreate a healthier society.
COVID CARE provides us a model in which to move forward together.
Container: Who is in your current social circle?
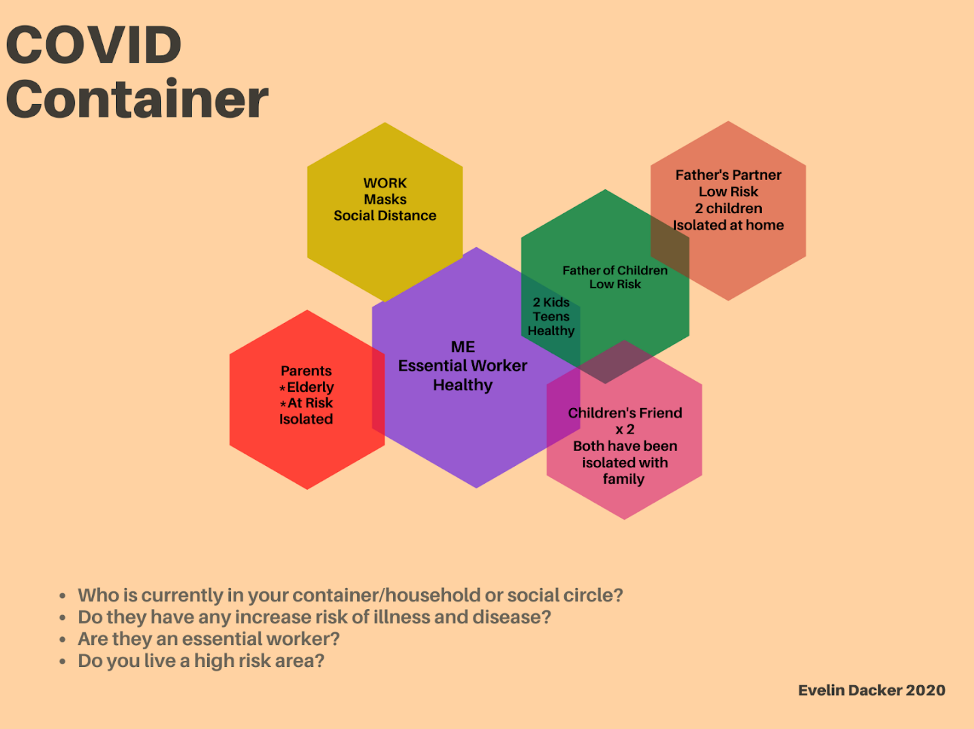
The Container includes the people who are in your household/domicile, living space, work space, or whom you might interact with without social distancing or precautions.
You could have a primary container—those who you share space with—and a secondary container, such as work spaces or visitors who have their own primary residences or containers. Those with bigger containers have bigger risks of infections associated with them.
Your container can have people at different social distances and include people who are in multiple containers. It should include the people who you directly intersect with: anyone who comes within six feet of you for more than 10 minutes. As time goes on, these containers may change, with people moving away or closer.
While it may seem like a hassle, drawing out your contacts can be a visual way to show others. This way, others can better make a decision knowing who is who and what they are willing to enter.
Many people know who is in their container, and feel safe within those choices, but many people do not have that privilege. Essential/front line workers, incarcerated, houseless, and people in detention, have no say or ability to protect themselves from viral transmission. We have a social responsibility to them to understand our ability to make choices and continue to account for this when we begin to open up our container to others.
You can create your own Container diagram here to share with others.
Agreements: What agreements that you have with the people in your current container?
We often take people who we live with for granted. Maybe we have not clearly sat down and spoken our boundaries and risk reduction etiquette out loud, but have a common understanding of each other while we are in the place of “stay at home” measures. As we move toward broadening our containers, we need to create agreements with each other to help navigate these changes.
Agreements may have allowances for those not at the same level. For example, if one person in the container socializes with others at less than six feet, the other members of the container may wish to stay more than six feet from them, and ask for extra cleaning of shared spaces or wearing of masks when near each other. The highest risk person or the person with the lowest risk tolerance would ideally set the standards of acceptable behavior for the container.
In some containers, it is difficult to have perfect risk reduction behaviors, such as maintaining six-foot distance from strangers, wearing masks, or staying at home. In these situations, disclosure about the additional risks to others must be made as one broadens the social network. This is not about getting an infection that can easily be treated with an antibiotic, but something that can kill someone even with two degrees of separation.

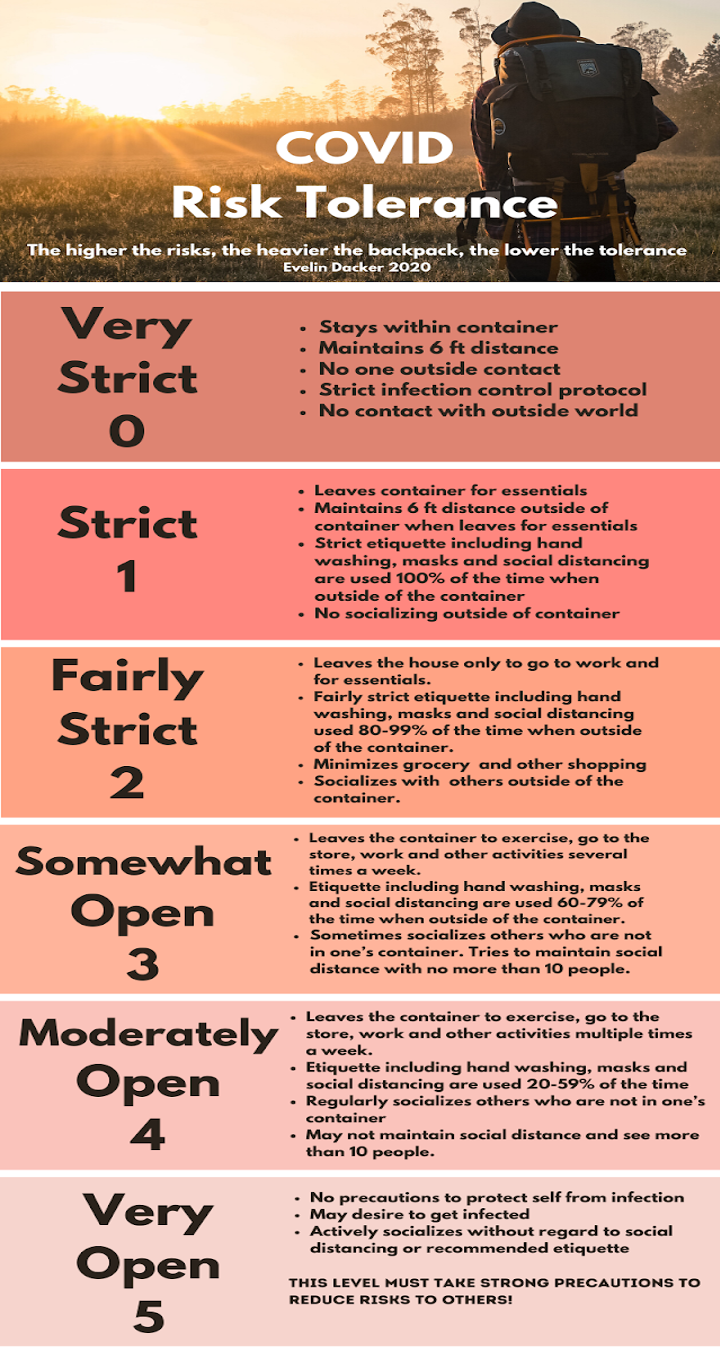
Risk tolerance: What is your tolerance for risk for yourself and what are you putting onto others?
This is the most controversial and difficult place to navigate as we reduce social distancing and open society back up. Forsaking joy, love, pleasure, and others for the period of time until herd immunity is reached will cause inordinate suffering. We each have our own personal tolerance for illness, disease, and death.
It is imperative that we understand this in order to take into account everyone else in our container and community at large. Risk Tolerance does not supersede public health policies and government regulations.
Why consider risk tolerance and not just risks themselves?
Risk tolerance is subjective and can dictate the behaviors we impart unconsciously to others. We each form our risk tolerance based on personal history and societal risks. Understanding risk tolerance and being responsible for your choices is critical to our ability to open up our society as safely as possible.
Low or high risk tolerance does not make one better or worse, but with COVID-19, the need to be clear and conscious with one’s choices is critical to the health of society.
The more someone is at risk of disease and death due to where they live, their health, pre-existing conditions, economic status, race, or age, the lower their risk tolerance. Others feel that they have less to lose if they get sick, and are willing to take on more risks. One cannot know everyone’s level of vulnerability who we come in contact with. Essential workers and those they care for have died due to others’ inadvertent exposure.
I use a backpack as a metaphor to explain the concept of risk tolerance:
The more you carry in your backpack (personal risks, precautions you are using), the slower you move (lower tolerance), but the more likely you are to survive. The less you carry, the faster you move (high tolerance), but the less likely you will survive by putting yourself and others at higher risk.
As risk tolerance increases, so does the potential harm to others. You are responsible for protecting others from yourself, otherwise that is a consent and boundary violation.
Higher risk front line and essential workers, people of color, migrant workers, and those residing in nursing homes are at especially high risk and may not have the ability to protect themselves with this conversation, so it is up to those of us who can, to help everyone stay healthy.
The following scale is not inclusive of all situations and is just a guide. This is not prescriptive. The intent here is to create a common vocabulary so we can communicate where we each stand.
0: Very Strict—Have been in very strict isolation alone or with others in a container.
People in this category are more likely to be at a higher risk of death from contracting the disease or be in a container with someone who is. They may value social responsibility toward others, and/or want to flatten the curve.
Areas with a high density of people, such as a city, may be at this level for the foreseeable future, until adequate testing and contact tracing is readily available. Getting through this pandemic without illness to self or others is a strong priority.
1: Strict—Have been in strict isolation alone or with others in a container.
For some, while they may want to be at this level, they cannot due to their societal, economic, and/or personal situation. Essential workers may be strict when they are able to make those decisions but their work puts them at higher risk, so their risk tolerance is higher than their desire.
2: Fairly Strict—Have been in fairly strict isolation alone or with others in a container.
People in this category may need more social exchange with others but still want to reduce the risks of infection as much as possible. Other circumstances, such as needing to continue work or take care of someone outside of the primary container, may require this level of risk tolerance.
3: Somewhat Open—Have chosen to be somewhat open with their container alone or with others.
People in this category may be found in places with lower COVID infections. Those who have lower risk of death and disease to themselves, and do not share space with others at high risk, may be in this category.
4: Moderately Open—Have chosen to be moderately open with their container alone or with others.
People here may believe they have no risk factors, or do not believe they know anyone who is at risk if they get the infection, or may be wanting to get infected.
They may have already been infected, tested positive for antibodies, and feel sure that they are no longer a vector for infecting others. Please note, that at the time of this writing, we do not know whether having antibodies to SARS-CoV-2 imparts immunity.
5: Very Open
Some people desire infection, have tested positive for antibodies, or do not want to be told what to do.
Anyone with this risk tolerance has the social responsibility to take strong precautions from possibly infecting others who may be vulnerable, including essential workers.
Etiquette: What code of socially responsible behaviors do you agree to?
As members of a greater community, the choices we make will help support one another. Some of these choices are based on hard science, such as handwashing protocols. Others we are still figuring out, such as the benefits of wearing masks.
Clean hand protocol. Wash your hands often with soap and water for at least 20 seconds, especially after you have been in a public place, or after blowing your nose, coughing, or sneezing.
If soap and water are not readily available, use a hand sanitizer that contains at least 60 percent alcohol. Cover all surfaces of your hands and rub them together until they feel dry.
Avoid touching your eyes, nose, and mouth with unwashed hands.
Secure shared space: Determined by those within a container. This may be a place where you do not feel the need to have strict measures such as wiping down surfaces after touch, wearing gloves, or covering your face.
Physical (social) distance: six feet is an old determination that has been the set standard for shared air space. Previous studies, using aircrafts as a model, have determined that this is the distance needed to avoid sharing small droplets. However, a sneeze or cough can carry viral particles much further.
Covering your coughs and sneezes: All coughs and sneezes, even if they are due to environmental allergies, need to be covered. The ideal is a clean paper tissue that is immediately thrown away into a closed container. Hands need to be washed or use of hand sanitizer immediately afterwards.
Masks: Are worn to protect others from you, not the other way around. Wearing a mask in public can have an overall impact of slowing down the transmission of the virus. The CDC does recommend the use of a mask, even a plain cloth mask, whenever you are out in public. If everyone was to wear a mask in public, it reduces the inadvertent transmission of people who may be asymptomatic as well. Please remember to wash your cloth masks regularly.
See this New York Times article for further information: A User’s Guide to Face Masks
Gloves: Are not well recommended since some people use the wearing of gloves to touch anything. Gloves can give a false sense of protection. If you are going to wear gloves, they must be put on after a 20-second handwash or use of alcohol sanitizer.
Do not touch your face with your gloved hand or you will self-contaminate. Take off the gloves as soon as they are no longer needed. Pull one off first, then use the clean hand to go under the glove to pull the other one off. Do not reuse them and dispose of them in a closed container.
Sex: The virus lives in saliva, any exchange of bodily fluids carries a risk of transmission. The virus has been found in stool, so any anal play can transmit the virus to your respiratory passages (mouth) and should be avoided unless you are in a mutually monogamous container with them.
Sexual activity is not limited to exchange of bodily fluids and this might be a chance to discover the array of sensual and intimate activities that are available to us.
Conclusion
We are in a time of great uncertainty. We do know, for those that believe in data and science, that social distancing, adequate handwashing, and stay at home measures have reduced the transmission of SARS-CoV-2 virus. Until accurate testing is widely available and contact tracing set up, these are the best measures we have to decrease morbidity and mortality due to COVID-19.
Unfortunately, there isn’t a clear end in sight.
Rather than despair, we need to find a way to proceed forward with grace and compassion. Communication with those in your day-to-day life, having clear agreements to meet everyone’s needs, and understanding your conscious and unconscious behavior will be critical as we begin to open up our society.
Until we have what we need to safely relax social restrictions, talking with those in your container/circle is one small tool that can go a long way as we prepare to ride out this storm together. Shame has no role in helping us stay together. Rather than using shame as a tool to encourage conformity, I recommend using accountability and communication.
Using COVID CARE as a model for communication, each can work toward creating a new “normal” where we learn to be self-aware, responsible, and care for one another.
~
More resources:
Facts on use of Face Masks
DIY Face Masks, NYTimes
CDC Mask Recommendations
The History of Social Distancing, NYTimes
Social Distancing, NYTimes
CDC Prevention Recommendations





Read 1 comment and reply