Editor’s Note: This website is not designed to, and should not be construed to, provide medical advice, professional diagnosis, opinion, or treatment to you or any other individual, and is not intended as a substitute for medical or professional care and treatment.
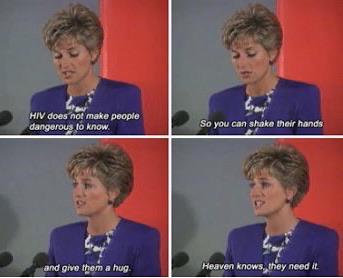
Bonus: “wonderful words from a wonderful woman.”
And also about how to cope with and help the people who have it.Not only do we have amazing treatments for HIV, we now have PrEP. A drug to take daily, and it near perfectly prevents you to get HIV through any form of sex (70% prevention through shared needles).
It is highly recommend that most gay men and other higher risk individuals take it so we can stop this epidemic.
San Francisco is an interesting case study. Once the epicenter of new HIV cases, they’ve aggressively embraced PrEP and actually have a chance to virtually eliminate new cases on the path they’re on.” ~ reddit comments.

My Partner is HIV Positive. {Adult}
“I have something I need to tell you.”
These are not words I want to hear, pretty much ever, but especially not when naked, horny, and from the mouth I had just been kissing.
“I am HIV positive.”
And my mind goes, “dying-children-in-Africa-Tom-Hanks-balding-dying-super-skinny.”
That was over a year ago. My partner, whose mouth I continued to kiss, and I have navigated many complicated landscapes since then, both emotional and physical. I am sharing my experiences with the hope of educating people and mitigating the stigma that still exists around HIV.
So how does stigma manifest?
Let’s start at the beginning: the moment of disclosure, “outing yourself” as HIV positive. The reactions attached to this are symptoms of stigma. I set myself as a “shining” example. Back to our earlier conversation:
“I am HIV positive.”
“Errrr. Wow. Okay. Wow. Well, errr, okay, I need to think about this before we have sex.”
No, “Thank you for telling me,” no, “Okay, and how do you deal with it?” no, “I’m so sorry, but I heard it’s not such a problem. Are you on antiretrovirals that make you undetectable and therefore unable to pass it on?”
Instead, he feels rejected. He feels ostracized. I feel scared and prejudiced and disappointed even. Disappointed that I can’t have sex anymore with this super-hot guy because I’m going to get sick if I do. Aren’t I?
Can I have safe sex with someone who has HIV? The answer, resoundingly, is: “Yes.”
Firstly, we have our age-old, Vatican-approved method: condoms.
They provide excellent protection against most STDs and the same goes for HIV—we all know this. But I was still nervous. What if the condom breaks? What if it comes off? What is safe sex? My scared mind immediately answered this question, “Safe sex means sex with a condom. Not sex with someone with HIV.”
It is still a commonly held belief that HIV positive people are a risk to the rest of us. “They” could infect “us.” It’s often not true anymore.
Modern medicine means that to be HIV positive today equates to having a chronic disease and to taking medication every day. This meditation makes you unable to transmit HIV, capable of having children without infecting your partner or the child, and living a long and healthy life.
Triumeq, Eviplera, Odefsey, Genvoya, Atripla, Stribild; all of these pills are available and on the market as anti-HIV drugs licensed for use in the European Union. To understand how, we need to educate ourselves briefly on what it means biologically to have HIV and how that affects your blood.
Science part, you ready?
HIV is a virus, specifically a retrovirus which means that it inserts a DNA copy of its genome into the host cell in order to replicate. It becomes part of your cells, rather than a normal virus which temporarily “takes over.”
Your viral load is how many particles of HIV are in your blood. If you get HIV in Germany, and you go to the doctor, you get prescribed antiretroviral medication (ART). This medication works to reduce the amount of HIV in your blood.
If your viral load is below a certain number, and you have tested over a period of time (recommended six months), then the HIV is still present but undetectable. When it is undetectable, you cannot infect anyone else. Not with blood, not with sperm, just not.
My reaction to my partner’s disclosure represents one of the modern cornerstones of stigma surrounding HIV.
If I had known then what I’m telling everyone here, I wouldn’t have had the same reaction. If more of us knew, perhaps stigma would cease to exist.
Why was I unaware? How is it that I did not know this information? I’m 33, I’ve had plenty of sex, I’ve traveled all over the place, I had sex-ed in school, and I’ll happily talk sex with all my friends. What’s more, I am entrenched in the BDSM community in Berlin and regularly attend events and workshops on sexuality, gender, and conscious BDSM.
My friends from this and other groups are of all ages, genders, and sexualities—and yet, I heard “HIV” and thought, “Ahhhhhh, Philadelphia.” It worries me that I am not simply the one clueless idiot, but I represent the vast majority.
When I looked deeper into it, within both social communities, conscious sexuality communities, and within the medical profession, I found that hardly anyone apart from the specialists are up to date on any of this. Information is not getting through.
Is this information all out there and freely available? In Germany, the specialist HIV organisations are the Deutsche AidsHilfe and Berliner AidsHilfe where information on ART therapy (in German Schutz-therapie) can be found. In the U.K., the specialist organistion is the Terrence Higgins Trust. They have a strong campaign called “Can’t pass it on,” which firmly states:
“Medical evidence has shown that people on effective HIV treatment can’t pass it on.”
But the main body of knowledge and reference for the U.K. is, as ever, the National Health Service (NHS). And what is the NHS saying?
“For people with HIV, taking effective HIV treatment and being undetectable significantly reduces the risk of passing HIV on to others.”
When you dig further into the “prevention” page, there is no mention of Terrence Higgins’ “effective HIV treatment” (ART).
The information regarding how to deal with HIV transmission differs depending on the type of doctor and country of location.
I realised that the information simply has not yet trickled down sufficiently within the medical profession. Responses and advice are disjointed and outdated.
They are much more advanced on the topic in Germany for example, than in the U.K. Over the last year, my visits to different doctors in different countries left me with a feeling of insecurity and uncertainty, as well as causing unnecessary strain on my relationship.
When I go to my partner’s HIV specialist, I am told that we do not need to use condoms and that there is no risk because he takes his HIV medication regularly and his viral load is below the required level, making him undetectable.
When I visit the Berliner AidsHilfe in Berlin, they tell me the same. When I visit a normal doctor or GP, and when I go to the sexual health clinic, in the U.K., and in Germany, I am recommended to both use condoms and take PrEP, a medicine which blocks me from being able to contract HIV.
When I look online, the NHS and even AidsMap are not outright supporting the specialists’ stance. Instead, they go for something much more reserved:
“It may be reassuring to know that you can have a long-term relationship and a fulfilling sex life with your partner, and stay HIV negative. It’s completely safe to kiss and hug your partner. Using condoms is a very effective way of preventing HIV transmission during sex. If your partner is taking HIV treatment and has an undetectable viral load, this also reduces the risk of transmission to a negligible level.”
One friend commented suggestively, “Putting a lot of faith there in modern medicine.” Perhaps he is right? I certainly thought about it; what if the medication fails? What does the medication do even? How often has that happened? Where is the evidence? So, for all of you who want the specifics, here you go.
Vernazza in 2008 was the first doctor to confirm that, “An HIV-infected person on antiretroviral therapy with completely suppressed viremia (“effective ART”) is not sexually infectious, i.e. cannot transmit HIV through sexual contact.”
This caused a huge reaction in the medical community who were reticent if not outright opposed to taking on this new evidence in the following years. It has become the go-to study and statement for modern approaches toward HIV care and prevention, either as a reference point, or still, at times, as a point of consternation.
The study itself took place over 14 years and looked at 393 heterosexual couples where one of the pair was HIV positive and the other not (also known as sero-different couples). You can read it in English here and the original here (in French).
The next most well-known and heavily referenced study was the PARTNER study, conducted between 2010 and 2014, published only in 2016, looking at heterosexual couples and men who have sex with men (MSM). It involved 1,166 couples, followed each couple up around one year later, and found zero documented cases of within-couple HIV transmission.
Other studies include:
>> This one, with 541 men observed over four years, which shows that when on ART, HIV is negligible even in the pre-ejaculate.
>> HTPN052, which emphasises the importance of taking up antiretrovirals early after diagnosis to significantly reduce the likelihood of infecting others.
>> This one, which explains the role of viral load in HIV transmission.
>> This one from 2009 which supports the Vernazza 2008 statement by stating, “Studies of heterosexual discordant couples observed no transmission in patients treated with ART and with viral load below 400 copies/ml” but calls for further investigation and data.
I firmly support condom use.
The campaign for the use of condoms has been essential to curb and continue to prevent the spread of HIV and other STDs, let’s not forget about those, please.
The feeling, however, is that the medical community is reticent to adopt a new position on recommendations for condom use because the fear is that people will see it as a green light for unprotected sex.
Although I don’t think everyone would throw off the Durex and scream “orgy” like that’s all that was preventing us from rutting in the streets, but it’s undeniable that complacency would creep in.
I therefore also support and promote the furthering of the discourse around HIV transmission and prevention and the firm appropriation of decade-old, strong, medical proof on the advancement of anti-retroviral therapies (ART) and their effectiveness as a chemical barrier which prevents the transmission of HIV.
Condoms work. Antiretroviral medication works.
Someone who is HIV positive taking ART treatment consistently for over six months, who is checked regularly and is aware that their viral load is undetectable, and who has no other STDs, is extremely unlikely to transmit HIV to their partner.
Stigma is quoted repeatedly as one of the central issues for people who are HIV positive. If people with HIV were not so afraid of being shunned or rejected or demonized for their status, they would feel safer to disclose.
The only way of combating this stigma is through education.
Relephant Reads:
What is it Like to Have Herpes?
How to talk about Sexually Transmitted Infections, minus the Shame.
Author: Rebecca Jackson
Image: With the permission of Johannes Wewetzer
Editor: Sara Kärpänen
Copy editor: Yoli Ramazzina


Read 2 comments and reply